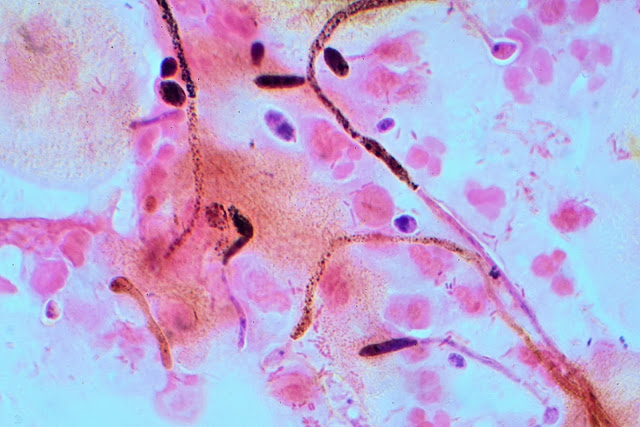
Thrush, also known as candidiasis, is a fungal infection caused by an overgrowth of the Candida fungus. Candida is a type of yeast that naturally lives in our bodies, including the mouth, throat, and...
Showing posts with label Health. Show all posts
Showing posts with label Health. Show all posts
CHRIMT
What Is Dry Eyes: Causes, Treatment and Prevention
Dry eyes, also known as dry eye syndrome, is a common condition that occurs when the eyes do not produce enough tears or the quality of the tears is poor. Tears play an important role in lubricating...
CHRIMT
Leukoplakia: Causes, Symptoms and Treatment
Leukoplakia is a medical condition that involves the development of thick, white patches or plaques on the mucous membranes lining the mouth, throat, or tongue. These patches can also occur on the genitals,...
CHRIMT
What Is Chiari Malformation
Chiari malformation is a condition in which the cerebellum, which is the part of the brain responsible for coordination and balance, extends into the spinal canal. This can cause compression of the brainstem...
CHRIMT
Brain Tumor-Causes, Symptoms and Treatment
A brain tumor is an abnormal growth of cells within the brain or surrounding tissue. Brain tumors can be either benign (non-cancerous) or malignant (cancerous), and they can arise from different...
Subscribe to:
Posts (Atom)